Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Impact of Post-Transplant Diabetes Mellitus on Survival and Cardiovascular Events in Kidney Transplant Recipients
- Ja Young Jeon, Shin Han-Bit, Bum Hee Park, Nami Lee, Hae Jin Kim, Dae Jung Kim, Kwan-Woo Lee, Seung Jin Han
- Endocrinol Metab. 2023;38(1):139-145. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1594
- 1,674 View
- 120 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Post-transplant diabetes mellitus (PTDM) is a risk factor for poor outcomes after kidney transplantation (KT). However, the outcomes of KT have improved recently. Therefore, we investigated whether PTDM is still a risk factor for mortality, major atherosclerotic cardiovascular events (MACEs), and graft failure in KT recipients.
Methods
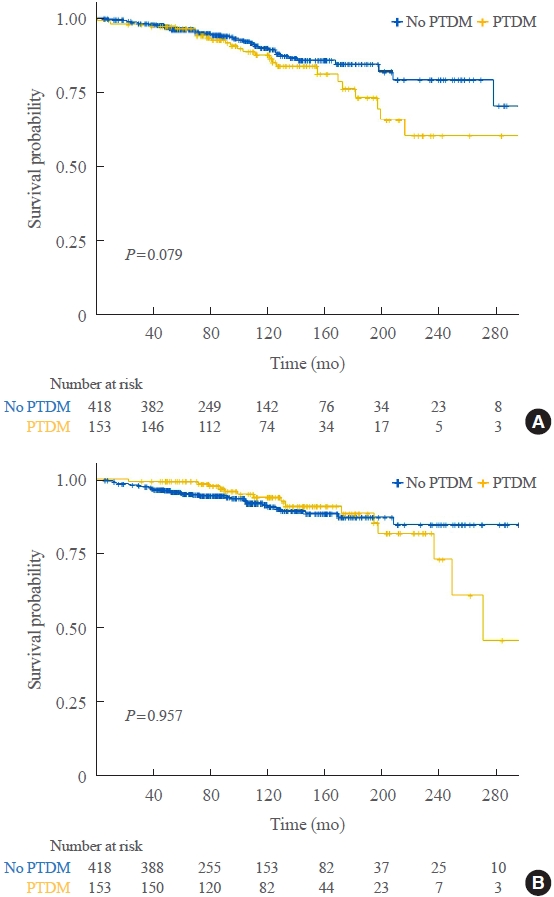
We studied a retrospective cohort of KT recipients (between 1994 and 2017) at a single tertiary center, and compared the rates of death, MACEs, overall graft failure, and death-censored graft failure after KT between patients with and without PTDM using Kaplan-Meier analysis and a Cox proportional hazard model.
Results
Of 571 KT recipients, 153 (26.8%) were diagnosed with PTDM. The mean follow-up duration was 9.6 years. In the Kaplan- Meier analysis, the PTDM group did not have a significantly increased risk of death or four-point MACE compared with the non-diabetes mellitus group (log-rank test, P=0.957 and P=0.079, respectively). Multivariate Cox proportional hazard models showed that PTDM did not have a negative impact on death or four-point MACE (P=0.137 and P=0.181, respectively). In addition, PTDM was not significantly associated with overall or death-censored graft failure. However, patients with a long duration of PTDM had a higher incidence of four-point MACE.
Conclusion
Patient survival and MACEs were comparable between groups with and without PTDM. However, PTDM patients with long duration diabetes were at higher risk of cardiovascular disease. -
Citations
Citations to this article as recorded by- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study
Uğur Ünlütürk, Tolga Yıldırım, Merve Savaş, Seda Hanife Oğuz, Büşra Fırlatan, Deniz Yüce, Nesrin Damla Karakaplan, Cemile Selimova, Rahmi Yılmaz, Yunus Erdem, Miyase Bayraktar
Endocrine.2024;[Epub] CrossRef - Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Safety and efficacy of semaglutide in post kidney transplant patients with type 2 diabetes or Post-Transplant diabetes
Moeber Mohammed Mahzari, Omar Buraykan Alluhayyan, Mahdi Hamad Almutairi, Mohammed Abdullah Bayounis, Yazeed Hasan Alrayani, Amir A. Omair, Awad Saad Alshahrani
Journal of Clinical & Translational Endocrinology.2024; 36: 100343. CrossRef
- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Drug Repositioning Using Temporal Trajectories of Accompanying Comorbidities in Diabetes Mellitus
- Namgi Park, Ja Young Jeon, Eugene Jeong, Soyeon Kim, Dukyong Yoon
- Endocrinol Metab. 2022;37(1):65-73. Published online February 8, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1275
- 3,785 View
- 164 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
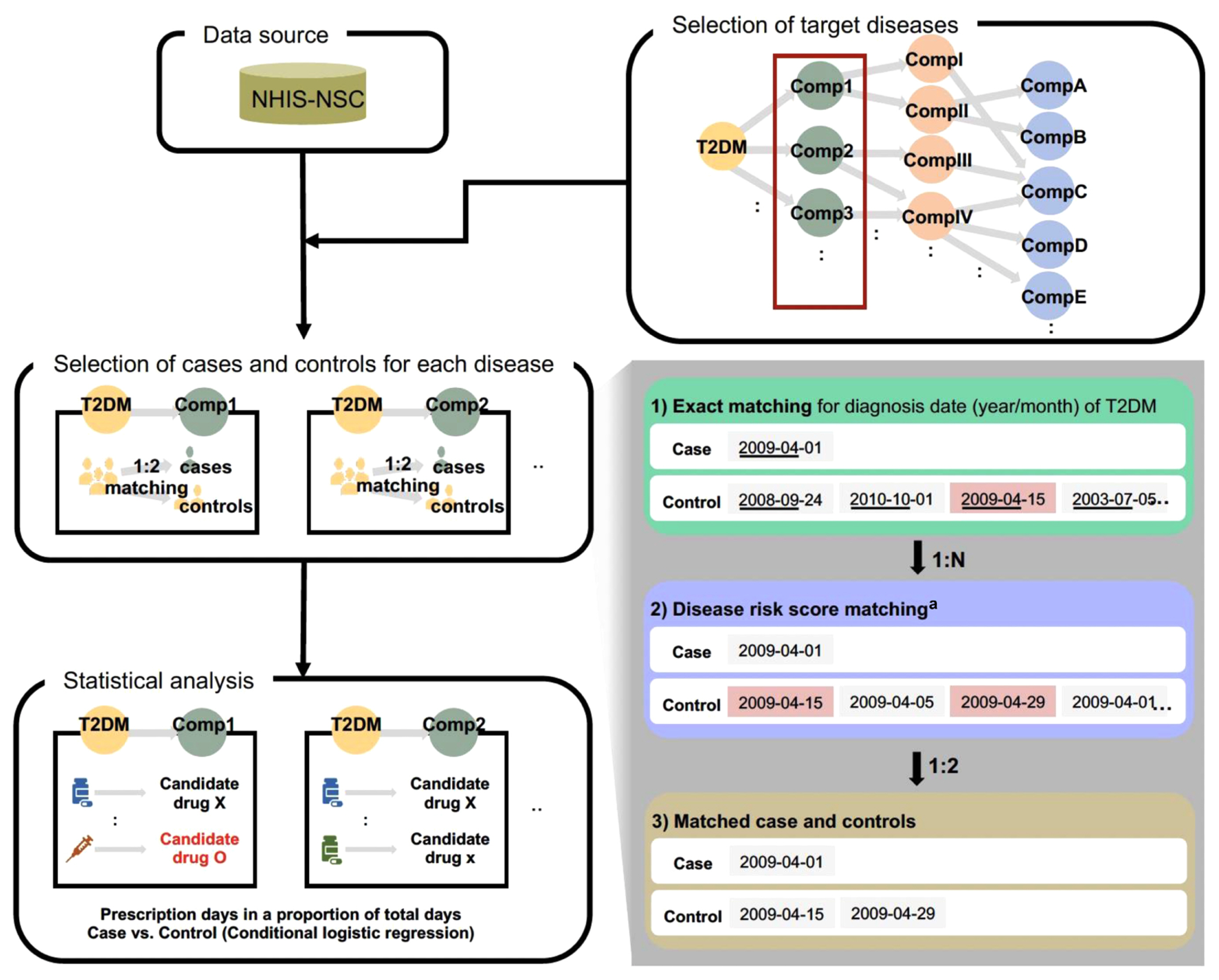
Most studies of systematic drug repositioning have used drug-oriented data such as chemical structures, gene expression patterns, and adverse effect profiles. As it is often difficult to prove repositioning candidates’ effectiveness in real-world clinical settings, we used patient-centered real-world data for screening repositioning candidate drugs for multiple diseases simultaneously, especially for diabetic complications.
Methods
Using the National Health Insurance Service-National Sample Cohort (2002 to 2013), we analyzed claims data of 43,048 patients with type 2 diabetes mellitus (age ≥40 years). To find repositioning candidate disease-drug pairs, a nested case-control study was used for 29 pairs of diabetic complications and the drugs that met our criteria. To validate this study design, we conducted an external validation for a selected candidate pair using electronic health records.
Results
We found 24 repositioning candidate disease-drug pairs. In the external validation study for the candidate pair cerebral infarction and glycopyrrolate, we found that glycopyrrolate was associated with decreased risk of cerebral infarction (hazard ratio, 0.10; 95% confidence interval, 0.02 to 0.44).
Conclusion
To reduce risks of diabetic complications, it would be possible to consider these candidate drugs instead of other drugs, given the same indications. Moreover, this methodology could be applied to diseases other than diabetes to discover their repositioning candidates, thereby offering a new approach to drug repositioning. -
Citations
Citations to this article as recorded by- Drug Repositioning: Exploring New Indications for Existing Drug-Disease Relationships
Hun-Sung Kim
Endocrinology and Metabolism.2022; 37(1): 62. CrossRef
- Drug Repositioning: Exploring New Indications for Existing Drug-Disease Relationships

- Clinical Study
- Insulin Secretion and Insulin Resistance Trajectories over 1 Year after Kidney Transplantation: A Multicenter Prospective Cohort Study
- Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Su Hyung Lee, Ja Young Jeon
- Endocrinol Metab. 2020;35(4):820-829. Published online November 18, 2020
- DOI: https://doi.org/10.3803/EnM.2020.743
- 4,953 View
- 119 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated the changing patterns of insulin secretion and resistance and risk factors contributing to the development of post-transplant diabetes mellitus (PTDM) in kidney recipients under tacrolimus-based immunosuppression regimen during 1 year after transplantation.
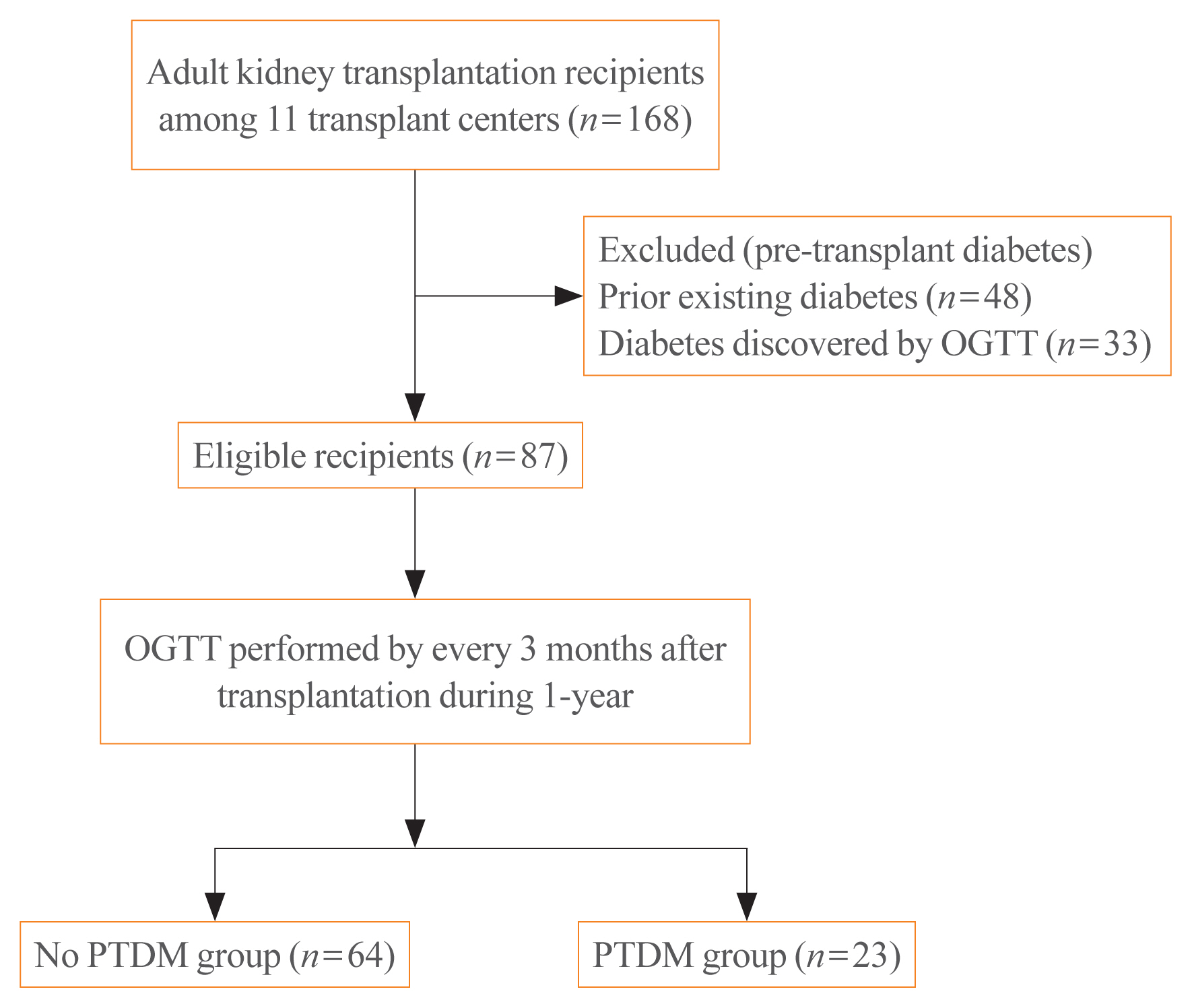
Methods
This was a multicenter prospective cohort study. Of the 168 subjects enrolled in this study, we analyzed a total 87 kidney transplant recipients without diabetes which was assessed by oral glucose tolerance test before transplantation. We evaluated the incidence of PTDM and followed up the index of insulin secretion (insulinogenic index [IGI]) and resistance (homeostatic model assessment for insulin resistance [HOMA-IR]) at 3, 6, 9 months, and 1 year after transplantation by oral glucose tolerance test and diabetes treatment. We also assessed the risk factors for incident PTDM.
Results
PTDM developed in 23 of 87 subjects (26.4%) during 1 year after transplantation. More than half of total PTDM (56.5%) occurred in the first 3 months after transplantation. During 1 year after transplantation, insulin resistance (HOMA-IR) was increased in both PTDM and no PTDM group. In no PTDM group, the increase in insulin secretory function to overcome insulin resistance was also observed. However, PTDM group showed no increase in insulin secretion function (IGI). Old age, status of prediabetes and episode of acute rejection were significantly associated with the development of PTDM.
Conclusion
In tacrolimus-based immunosuppressive drugs regimen, impaired insulin secretory function for reduced insulin sensitivity contributed to the development of PTDM than insulin resistance during 1 year after transplantation. -
Citations
Citations to this article as recorded by- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Distúrbio do eixo hipotálamo-hipófise-gonadal e sua associação com resistência à insulina em receptores de transplante renal
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Hypothalamic-pituitary-gonadal axis disturbance and its association with insulin resistance in kidney transplant recipients
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Postoperative fasting plasma glucose and family history diabetes mellitus can predict post-transplantation diabetes mellitus in kidney transplant recipients
Le Wang, Jin Huang, Yajuan Li, Kewei Shi, Sai Gao, Wangcheng Zhao, Shanshan Zhang, Chenguang Ding, Wei Gao
Endocrine.2023; 81(1): 58. CrossRef - Changes in glucose metabolism among recipients with diabetes 1 year after kidney transplant: a multicenter 1-year prospective study
Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Hyung Joon Ahn, Su Hyung Lee, Ja Young Jeon
Frontiers in Endocrinology.2023;[Epub] CrossRef - Pretransplant evaluation and the risk of glucose metabolic alterations after renal transplantation: a prospective study
Arminda Fariña-Hernández, Domingo Marrero-Miranda, Estefania Perez-Carreño, Antonia De Vera-Gonzalez, Alejandra González, Cristian Acosta-Sorensen, Ana Elena Rodríguez-Rodríguez, Tatiana Collantes, Marta del Pino García, Ana Isabel Rodríguez-Muñoz, Carla
Nephrology Dialysis Transplantation.2022;[Epub] CrossRef
- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis

- Obesity and Metabolism
- Testosterone Deficiency Associated with Poor Glycemic Control in Korean Male Diabetics
- Joo-Sung Kim, Bong Sun Kim, Ja Young Jeon, Yong Jun Choi, Yoon-Sok Chung
- Endocrinol Metab. 2014;29(3):300-306. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.300
- 3,516 View
- 31 Download
- 8 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have shown that men with diabetes have lower testosterone levels than healthy men. However, studies on the correlation between testosterone and diabetes are rare in Korea. We examined the relationship between testosterone deficiency and markers related to diabetes in adult Korean men.
Methods A total 464 men with diabetes who visited an outpatient clinic at Ajou University Hospital and had serum total testosterone and serum insulin levels measured between January 2000 and September 2013 were selected. Blood samples were collected after the subjects had fasted overnight. We divided the participants into testosterone deficient and normal groups. Testosterone deficiency was defined as having a serum total testosterone level <3.5 ng/mL.
Results Of 464 subjects, 34.9% had a testosterone deficiency. The mean levels of fasting plasma glucose (
P =0.007) and glycated hemoglobin (HbA1c;P =0.038) were significantly higher in the testosterone deficiency group than in the normal group. To clarify the relationship between serum total testosterone level and fasting plasma glucose or HbA1c values, Pearson's correlation test was performed. Fasting plasma glucose levels (r =-0.142,P =0.002) and HbA1c values (r =-0.097,P =0.040) showed a significant negative correlation with serum testosterone levels in men with diabetes.Conclusion Major markers of diabetes that are associated with testosterone deficiency are fasting plasma glucose and HbA1c values. Poor glycemic control appears to be associated with testosterone deficiency in Korean men with diabetes.
-
Citations
Citations to this article as recorded by- Association between T2DM and the lowering of testosterone levels among Kashmiri males
Rabia Farooq, Mohammad Hayat Bhat, Sabhiya Majid, Mohammad Muzaffar Mir
Archives of Endocrinology and Metabolism.2020;[Epub] CrossRef - Hypogonadism and associated risk factors in male patients with type 2 diabetes mellitus attending the diabetic clinic of Tikur Anbessa Specialized Teaching Hospital, Addis Ababa, Ethiopia
Sisay Teka, Samuel Kinde, Gobena Dedefo, Kissi Mudi, Getahun Tarekegn
Journal of Endocrinology, Metabolism and Diabetes of South Africa.2019; 24(1): 16. CrossRef - Hypogonadism in Nigerian men with type 2 diabetes mellitus
S. I. Onung, E. E. Young, T. E. Ugwu, O. A. Fasanmade
International Journal of Diabetes in Developing Countries.2017; 37(3): 254. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Association between T2DM and the lowering of testosterone levels among Kashmiri males

- Bone Metabolism
- Testosterone Replacement and Bone Mineral Density in Male Pituitary Tumor Patients
- Min Jeong Lee, Hyoung Kyu Ryu, So-Yeon An, Ja Young Jeon, Ji In Lee, Yoon-Sok Chung
- Endocrinol Metab. 2014;29(1):48-53. Published online March 14, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.1.48
- 3,523 View
- 33 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypopituitarism is associated with osteoporosis and osteopenia especially when hypogonadotropic hypogonadism is present. Despite hypopituitarism being an important cause of secondary osteoporosis, osteoporosis in patients receiving surgery for pituitary tumors in Korea has not been studied. In this study, we evaluated the effects of testosterone replacement therapy (TRT) on bone mineral density (BMD) in postoperative hypogonadal patients with pituitary tumors.
Methods To examine the effect of TRT on BMD, we performed a retrospective observational study in 21 postoperative male patients who underwent pituitary tumor surgery between 2003 and 2012 at the Ajou University Hospital. Testosterone was replaced in postoperative hypogonadal patients by regular intramuscular injection, daily oral medication, or application of transdermal gel. BMD (g/cm2) measurements of central skeletal sites (lumbar spine, femoral neck, and total femur) were obtained using dual-energy X-ray absorptiometry (GE Lunar). For lumbar spine BMD, L1 to L4 values were chosen for analysis. Femur neck and total femur were also analyzed.
Results During the follow-up period (mean, 56 months; range, 12 to 99 months) serum testosterone levels increased with the administration of TRT (
P =0.007). There was significant improvement (4.56%±9.81%) in the lumbar spine BMD compared to baseline BMD. There were no significant changes in the femur neck BMD or total femur BMD. We did not find any statistically significant relationships between changes in testosterone levels and BMD using Spearman correlation analysis.Conclusion Our results indicated that TRT used in the postoperative period for hypogonadal pituitary tumor surgery patients may have beneficial effects on the BMD of the spine.
-
Citations
Citations to this article as recorded by- Testosterone supplementation and bone parameters: a systematic review and meta-analysis study
G. Corona, W. Vena, A. Pizzocaro, V. A. Giagulli, D. Francomano, G. Rastrelli, G. Mazziotti, A. Aversa, A. M. Isidori, R. Pivonello, L. Vignozzi, E. Mannucci, M. Maggi, A. Ferlin
Journal of Endocrinological Investigation.2022; 45(5): 911. CrossRef - Physiological testosterone replacement effects on male aged rats with orchiectomy-induced osteoporosis in advanced stage: a tomographic and biomechanical pilot study
Vinícius de Paiva Gonçalves, Adriana Alicia Cabrera-Ortega, Jhonatan de Souza Carvalho, Dania Ramadan, Luís Carlos Spolidorio
The Aging Male.2021; 24(1): 139. CrossRef - Androgens and Androgen Receptor Actions on Bone Health and Disease: From Androgen Deficiency to Androgen Therapy
Jia-Feng Chen, Pei-Wen Lin, Yi-Ru Tsai, Yi-Chien Yang, Hong-Yo Kang
Cells.2019; 8(11): 1318. CrossRef - Testosterone and male rejuvenation
Sevann Helo, Peyton Thomas, Nicholas N. Tadros
Panminerva Medica.2019;[Epub] CrossRef - Systemic Non-Reproductive Effects of Sex Steroids in Adult Males and Females
Syed Imran Ali Shah
Human Physiology.2018; 44(1): 83. CrossRef - Benefits and Health Implications of Testosterone Therapy in Men With Testosterone Deficiency
Abdulmaged M. Traish
Sexual Medicine Reviews.2018; 6(1): 86. CrossRef - Multiple Fractures in Patient with Graves' Disease Accompanied by Isolated Hypogonadotropic Hypogonadism
Hyon-Seung Yi, Ji Min Kim, Sang Hyeon Ju, Younghak Lee, Hyun Jin Kim, Koon Soon Kim
Journal of Bone Metabolism.2016; 23(1): 40. CrossRef - Severity and pattern of bone mineral loss in endocrine causes of osteoporosis as compared to age-related bone mineral loss
D Dutta, P Dharmshaktu, A Aggarwal, K Gaurav, R Bansal, N Devru, UC Garga, B Kulshreshtha
Journal of Postgraduate Medicine.2016; 62(3): 162. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Bone health in hypogonadal men
Michael S. Irwig
Current Opinion in Urology.2014; 24(6): 608. CrossRef - Testosterone Replacement Therapy and Bone Mineral Density in Men with Hypogonadism
Se Hwa Kim
Endocrinology and Metabolism.2014; 29(1): 30. CrossRef
- Testosterone supplementation and bone parameters: a systematic review and meta-analysis study


 KES
KES

 First
First Prev
Prev



